Provider Credentialing
CureMB perceives that medical provider credentialing is a vital component of a healthcare facility’s operation. Our team of professionals maintain expertise in the provider credentialing process, including staying abreast of changes in the industry, credentialing trends, and payer requirements. As experts, we take on the credentialing process from start to finish. That means our team takes on all of the responsibilities that typically fall on your staff, freeing up your team to focus on more important tasks.CureMB can help you increase your credentialed payers, increase your patients, and maximize your market share. CureMB provider credentialing services ensure that your physician credentialing is completed correctly and timely. Our service offering includes Provider Credentialing, Medicare and Medicaid Enrollment, Insurance Contract Negotiations, Payer Fee Schedule Creation, and Telemedicine Credentialing. At CureMB, our team works with the provider to fill out the initial application, perform the due tasks required of the organization such as primary source verification, background screening, and coordinate with payers to support timely approval as well as expedite provider starts. All overseen by experienced, knowledgeable and professionals from the CureMB Team.
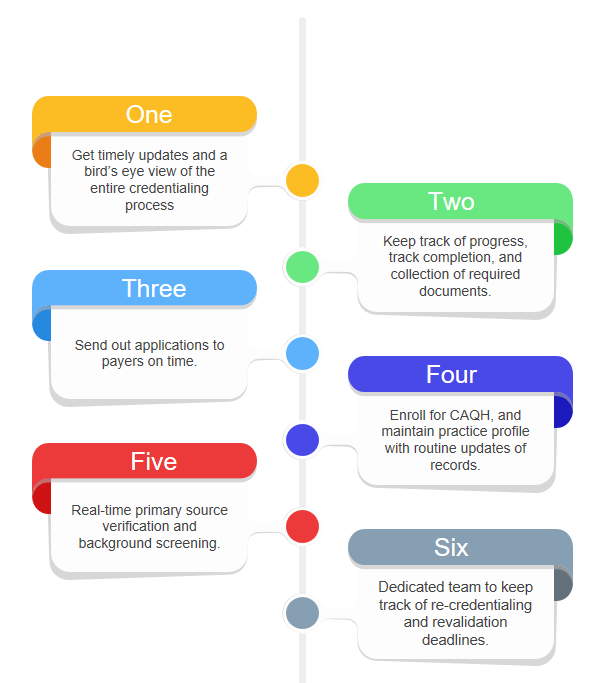
How we Monitor this: